by Guest | Apr 6, 2018 | Being Well
Early Childhood Development is a big deal. Many health, behavior and learning concerns can be addressed during the earliest years of childhood, setting the stage for a healthier, happier and more successful adult life. Because we don’t know what we don’t know, pre-natal care and annual well-child visits are key. It’s important to seek out professional guidance to optimize maternal and child health through appropriate nutrition and developmental interaction. Knowing which milestones to watch for during those critical first five years of a child’s life and receiving early intervention to address delays can be life-changing to a child.
Annual well-child visits to primary care providers may seem like a waste of time and money if a child appears to be developing normally but they are an opportunity to ensure both the family and the child have the resources they need to be successful. Providers and parents can consult the on-line “Ages and Stages” tool to assess a child’s progress. Talking with your child’s healthcare provider about behavior can also provide important information about a child’s development.
Home visits for pregnant and new moms are also available through the Tillamook County Community Health Centers and CARE’s Healthy Families program and provide a great way for families to learn ways to optimize their child’s development. Another great way to catch early developmental needs is through screenings. Children ages 2-6 can be seen at the annual Early Childhood Screening Fair, scheduled this year from April 18-20 at the Tillamook County Fairgrounds. At this FREE event, children receive 12 screenings including: Physical, Nutrition, Hearing, Vision, Child Development, Behavior, Dental, Speech and Lead. Families must call for an appointment: 503-815-2292. Door to door transportation can be made available upon request. There are many great parenting resources available to help ensure kids are developing on track. A fun tool called VROOM, which can be found on-line or as an App, provides free downloadable daily activity tips for parents with children ages 0-5. Every day, research-based, age appropriate tips are sent to mobile phones encouraging ‘brain-building moments’ between parents and their children. Each tip is easy to do and is customized for each child based on their age. Caregiver-child interaction plays a very large role in a child’s development. Vroom helps busy families incorporate brain-boosting moments into everyday activities.
Local parenting classes are also available. The next class is a 7-week long Active Parenting Class which will meet in South County on Tuesdays from 5:00-7:30 p.m., April 3 – May 15. Join other parents in learning about child development and what behavior to expect from your child at their age. You can also plan to increase your techniques to redirect bad behavior and re-duce stress in the family. Cost is $30.00 per adult and includes light dinner and materials. To learn more or to register, 503-842-8201 Ext 276 or JillV@tfcc.org.
YMCA to host Healthy Kids Day April 21
Healthy Kids Day is a national YMCA initiative to not only maintain but improve childhood health and well-being during the summer months. For so many school-age children, physical and cognitive activity and access to healthy food choices cease when the school year ends. Research shows that kids are prone to gain more weight and fall behind in studies when they don’t get up, get out, and grow during the summertime.
This year we are excited to partner with NW Parenting and bring back BlockFest, a research-based parent-child exhibit that raises awareness of science, technology, engineering, and math (STEM) by learning through play. Two decades of research show that children build number and math skills from a very early age, and that those who are strong in early math skills excel in math in the later years.
By establishing year-round healthy habits, families who play and eat healthy together take preventative measures against chronic diseases, such as Type 2 Diabetes. To aid in this effort, Tillamook YMCA kicks off the summer by inviting local community partners to participate in Healthy Kids Day and promote programs and activities that encourage health and well-being in both children and families. Participants can expect to play games, engage in activities, and learn about the valuable health and wellness resources Tillamook County has to offer.
All attendees will receive a raffle ticket to be entered into a drawing for some great door prizes, including admission to the Oregon Zoo and Sky High Sports Trampoline Park! Healthy Kids Day is a FREE event open to the public and will take place Saturday April 21st 10:00 am-1:00 pm in the YMCA gymnasium located at 610 Stillwell Avenue in Tillamook. For more information call (503)842-9622.

by Guest | Mar 23, 2018 | Being Well, Eat Well
By Laura Swanson
“I’ve been doing some research,” said Dr. Mark Bowman, Medical Officer at Adventist Health Tillamook Regional Medical Center, “And I can send you the studies,” he added, as we continued our conversation about why the Year of Wellness focus on type 2 diabetes prevention is so important. “The statistics are interesting and according to the research, having diabetes is equal to having heart disease,” Bowman stated. “The risk to your health is equal to having previously had a heart attack; that’s the impact that diabetes has on the body.” That’s why it’s important to control diabetes as it lowers the risk for complications.
As Dr. Bowman continues his practice of Functional Medicine, which focuses on the individual and finding the underlying causes for symptoms, ongoing and leading edge research provides a basis, but research is done with a tightly controlled group. “It’s almost impossible to replicate the conditions of a research group in reality,” explains Bowman. It’s an incomplete puzzle with different individual responses. Other systems that are impacted by diabetes, in addition to the increased risk for coronary disease are macro-vascular, kidney disease, retina deterioration, neuropathy, and hypertension.
Diabetes symptoms can be controlled with medication, but lifestyle changes are the “key and safest” medicine for slowing, and even reversing diabetes. “You can have a patient on insulin therapy for decades, but in most cases, the pancreas eventually loses the ability to continue producing high levels of insulin. Insulin resistance occurs at the cellular level,” explained Dr. Bowman.” It signals the body to increase fat cells and more insulin is required …it’s a vicious circle.” He continued, “When you make some simple lifestyle changes such as healthier eating and activity, you can delay and even reserve insulin resistance. It’s not easy for some people, and an individual approach is necessary.” That’s why Dr. Bowman is focusing on Functional Medicine. “It’s not a one-size-fits-all kind of medicine,” he added.
“The research is constantly being done and the findings continue to change our treatment options,” said Dr. Bowman, as he prepared to head to New York City for the Integrative Healthcare Symposium. “We are hearing more references to dementia and Alzheimer’s as ‘type 3’ diabetes,” said Dr. Bowman. “The impacts are micro-vascular and there is a link between reducing inflammation and improving systems functions. You can delay the progression with anti-inflammatory foods.” There it is again – “Food as medicine.” It’s more than an apple-a- day, according to Dr. Bowman, “Eat and drink as ‘clean’ as possible, reduce exposure to internal and external chronic stress. Seventy-percent of serotonin (the neurotransmitter chemical that impacts mood and more) is produced by the bacteria in the gut.”
Then there are those pesky genes and again how each individual’s systems function. One study looked at ways of reducing the complications of diabetes, with findings that an A1C level under 7 reduced onset of other chronic problems. It involved intensive lifestyle therapy, not medication. “There is current dialogue about diet and diabetics,” said Bowman. “Lower carb, plant-based. It’s all about reducing sugar, and carbohydrates and grains that metabolize into sugar.” Dr. Bowman was most looking forward to a presentation by Dr. Mark Hyman (A leader in Functional Medicine), “Food: What the Heck Should I Eat?” – which is also the title of his newest book. Our next interview with Dr. Bowman will be about the NYC symposium.
“We can continue to increase awareness and educate about lifestyle changes,” said Dr. Bowman. “encourage people to make healthier choices, develop particular ways and habits that have positive impacts on their quality of life.” He continued, “We get a label as diabetics, and internalize, suffering shame because ‘we must have done something wrong.’ By talking about diabetes, and many chronic diseases such as hypertension, lipid, and hormonal imbalances we can let people know there are ways to turn it around. Don’t suffer in silence, or simply, Band-aid with a pill.” He continued, “It’s an individual life journey and there’s a time and place for all tools. Increased awareness and acceptance of the different lasting options will ultimately help patients enjoy a satisfying life.”
by Guest | Mar 16, 2018 | Being Well
Two-for-one sales are always popular. We get twice as much for the cost of one. What if we can get a three-for-one deal? Wouldn’t that be awesome? In healthcare, this is referred to as the “Triple Aim.” Developed by the Institute for Healthcare Improvement, this framework sets a goal of improving population health, as well as quality of individual care, while at the same time reducing healthcare costs.
It may sound too good to be true, but great strides are being made to accomplish the Triple Aim. This isn’t just a good idea. It is necessary, given escalating rates of preventable illness and healthcare costs. Because the factors that influence health extend beyond the healthcare system, other sectors must become part of the “Triple Aim” solution. Government, schools, businesses, faith-based and civic organizations are just some of the partners that can help.
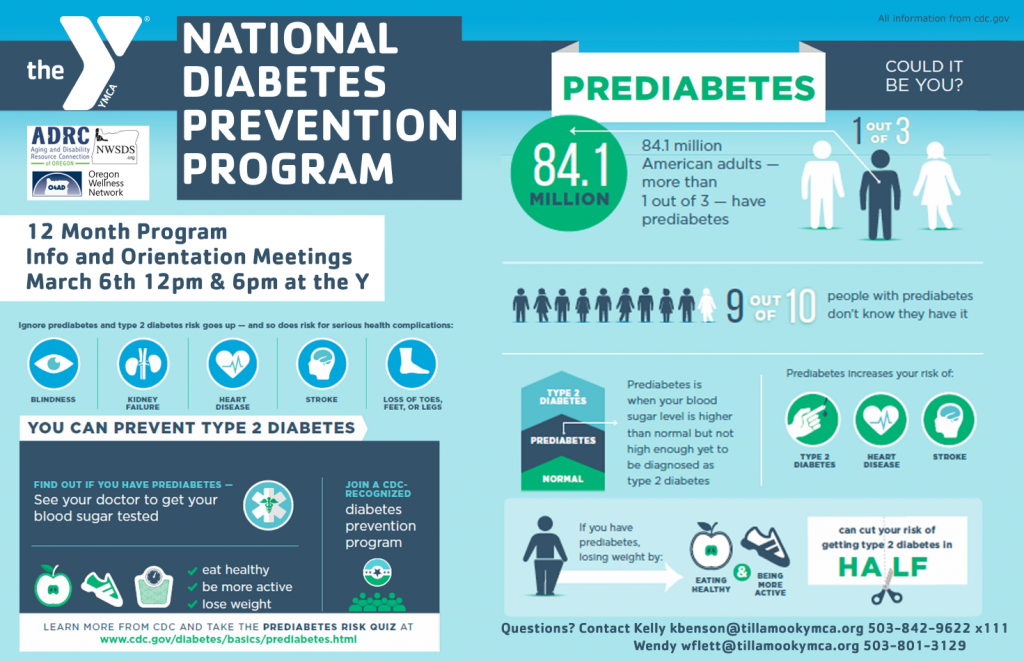
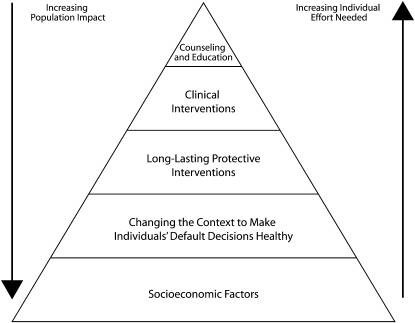
The Centers for Disease Control and Prevention (CDC) has developed the Health Impact Pyramid, a resource that helps communities understand how to get the best return on investment when working to improve population health. Traditionally, most of the time and money invested in helping people get or stay healthy happened at the top of the pyramid in the form of counseling, education and clinical interventions. While these are important strategies, they require more individual effort and often do not fully address the underlying, root causes affecting individual health.
Research has shown that investments in factors that influence a person’s education, employment and housing status, known as socioeconomic factors, can achieve a much higher rate of return. For example, community investment in early childhood development and care impact a child’s success in school and this will likely lead to a better job down the road. Education and employment status are associated with better health in adulthood.
The second level of the pyramid relates to making default choices healthier where people live, work and play. If we live close to a store that sells fruits and vegetables, we tend to eat more of those foods than someone who must travel a long distance to purchase them. Similarly, conveniently located sidewalks, bike lanes and trails make being active easier. Research shows that people who live in walkable communities are more active and healthier.
Continuous, paved pathways provide safe, accessible opportunities for all citizens to become more physically active. Currently, there are few places like this in Tillamook County. Kilchis Point Reserve, near Bay City, is a popular trail. Another good example is Bud’s Fitness Trail at Tillamook Junior High School. These paths allow people of all abilities to enjoy being active outdoors and accommodate strollers, walkers and wheelchairs. These off-road paths, such as the planned Crosstown Connections rail spur between Goodspeed Park & Hoquarton Slough, allow families with small children to recreate safely, even allowing a young child to skate, ride a bicycle or scooter – all important activities for physical development and social connectivity.
These paths are free to the public and open year-round. The return on investment comes from the increased health and community livability these resources provide. Development of the proposed Salmonberry Rail Trail within our coastal communities stands to not only generate significant economic development but also positive community health benefits.
The U.S. Surgeon General’s “Step It Up!” initiative encourages communities to invest in creating more walkable spaces near population centers. YOW partners are teaming up to highlight existing walking locations throughout Tillamook County. Community-based walking groups kick off the first week in April. Full details can be found on tillamookliving.com and will be featured in this column next week.

by Michelle | Mar 14, 2018 | Being Well
By Michelle Jenck, M.Ed., Certified Behavior Change Coach
Every day we hear the results of another study telling us “Eat this, don’t eat that,” or, “Move like this, not like that.” While it is good to learn about adopting healthier behaviors, it can be overwhelming to know where to start. Change is hard. Crazy hard. It’s really inconvenient. That’s how we got into this mess in the first place.
It is human nature to take the path of least resistance. It takes time and effort to change the way we live our lives. For most of us, this is where we end up – in a state of knowing we need to do something but not truly believing we are capable of doing it.
Being open to the possibility of changing is key. To be successful, we need to make the changes to our habits small, easy-to-adopt, and even enjoyable. Yes – that’s right. Change can be fun.
It helps to become aware of our habits and begin associating those with how we feel. How do I feel when I eat this and don’t eat that? How much energy do I have for daily activities? If the answers to these questions are not the ones you’d like, then it is probably time to start making some changes.
It is important to explore what is and isn’t working and examine what factors are in play. We tend to look only at the negative – what isn’t working. Looking at our “bright spots” may be a better option. What are we good at? When do we feel energetic? Happy? Fulfilled? How do we use this information to get more of that feeling in our life?
Why we want to make changes is almost as important as what we want to change. The “why” often determines our chances for success. If we are making a change for our spouse or boss, or as a quick fix (think high school reunion), we might not be as emotionally invested as we need to be successful over the long term.
Getting married and having kids are enormous life changes, yet, people make those changes every day. Maybe you want to see your kids or grandkids grow up. Maybe you want to improve your quality of life. Whatever it is, it needs to be meaningful to you.
Work with your strengths and interests when approaching change. If you like to cook, then it makes sense to find healthy recipes you would enjoy making. If you hate cooking, it will be important to simplify nutrition changes so that you can still be successful. Consider choosing the prepared veggie tray and a container of hummus from the grocery store.
This principle is especially important when it comes to physical activity. If you enjoy being outdoors, consider walking or hiking. If you like people, music and dancing, try a group fitness class. If you want something more mindful, try Tai Chi or Yoga. The key is to look for ways to integrate a positive, healthy change with your personality, interests and strengths.
Don’t worry about meeting some “ideal” behavior you saw on Pinterest or Facebook. The important thing is to start somewhere and start with something you like. It might not have to do with nutrition or fitness at all. Maybe you want to learn how to play the piano or knit. If the change is enjoyable and makes you feel better, you will be more likely to try new things later.
Adopting one new health habit successfully, no matter how small, usually leads to another and another. All this eventually opens a door to a much healthier, happier new you. And that’s the kind of change we can all get behind!

by Guest | Mar 2, 2018 | Being Well, Eat Well
By Sara Todd, LCSW, Rinehart Clinic
The shame experience is complex and holds a variety of feelings. Shame can be debilitating and all encompassing. Eye contact may feel painful, even impossible. At its worst, it can result in withdrawing from the world. A retreat into a darkness that feeds upon itself.
Shame is triggered by an external event and this can even include receiving the diagnosis of a medical illness, such as diabetes. The diagnosis may trigger shame because of feeling exposed as inadequate or incapable. A person may feel they don’t “measure up” to an ideal. The diagnosis can end up confirming what someone already feels about her or himself— that they are flawed or not good enough.
Shame has a social context and occurs in relationship with others. We will say, you shamed me. A tendency toward shame in one’s adult life may come from early experiences of being judged, ridiculed and not fully celebrated and enjoyed by one’s caregivers. This fundamental sense of “badness” repeats a cycle that originated in one’s early life. For some, shame may be a foundation underlying everything one does. Diabetes is just one more channel for that shame.
Shame thrives in darkness and loathes the light. Its antidote is radical acceptance, the full embrace of love and kindness by another and towards oneself.
Because diabetes intersects with a person’s relationship to their body, their relationship to food and eating and the authority of medical providers, it makes sense that all of this would trigger a shame response. The combination of society’s unrealistic beauty standards, feeling constantly “graded” through daily monitoring of blood glucose or A1c tests and the way we ignore the institutional reasons for challenges such as poverty and eating healthy, all contribute to an internal dialogue of “I did this to myself”.
What is the way out?
The first may be to have curiosity about the shame. Ask questions about the feeling and the storyline that you’re “not good enough.” Why do I feel ashamed about having diabetes? Open it up for exploration. If the shame is connected to not measuring up to an ideal version you have of yourself, you can ask: Who set that standard? Is this an ideal that comes from my own values or someone else’s?
Questioning the self-blame can also be effective. What may be other reasons I have this disease? Why else did it happen? Is there a family history, for example? The point is not to deflect accountability, but to bring a more complex understanding.
We can also begin to unravel this knot of humiliation, self-hate, and feeling outcast by “dropping the storyline.” When these thoughts “I’m not good enough…I did this to myself…I’ll never get it right” come up, take a deep breath, feel your body and then let the thoughts go. A teacher once gave me the tool of: Recognize-Refrain-Relax-Remain. Recognize that you are getting caught again in the feelings and thoughts of shame. Refrain from trying to escape the feelings (don’t numb out). Relax by deep breathing, stretching, taking a walk or simply just letting yourself be. And, finally, remain where you are in that moment. It will pass.
If shame is making it difficult to engage deeply with others and live your life fully, talking to a therapist may also be a good idea. Shame that originates in trauma needs healing with a licensed mental health professional. And as we heal the wound of shame, we begin to love ourselves more fully through the gift of improved health.
Most importantly, shed light on that shame because you, at your core, are good and perfect just as you are.
by Michelle | Feb 23, 2018 | Being Well, Eat Well
By Michelle Jenck, YOW Coordinator
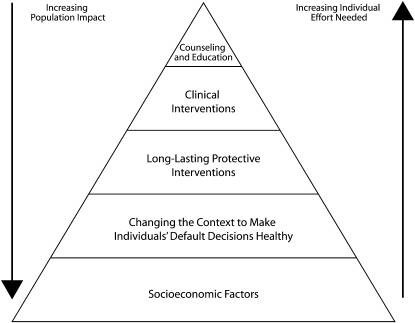
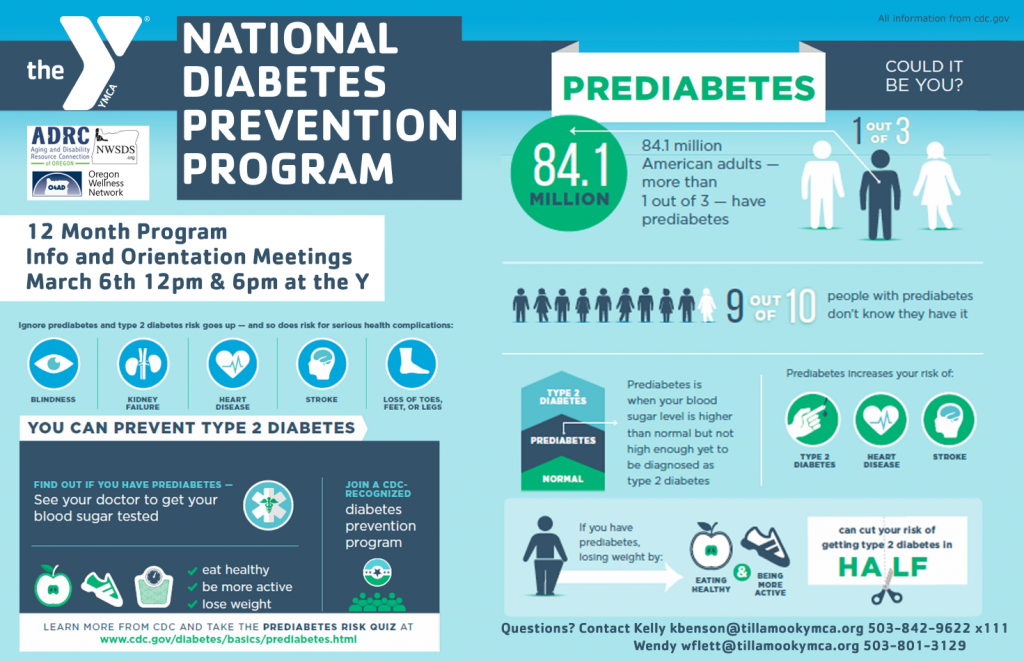
If it seems like you have been hearing a lot about diabetes and pre-diabetes lately, you are right. At the risk of over-sharing, the Year of Wellness team wants to make sure Tillamook County residents are getting the message – loud and clear. A lot of people have prediabetes and there IS something we can do about it.
Our YOW partners at the Y and Northwest Senior & Disability Services are teaming up to prevent diabetes in Tillamook County. This infographic highlights key risk factors and prevention methods. Losing even a few pounds (and keeping them off) can help most people reverse their risk of developing type 2 diabetes. The best way to do that is to follow healthier eating habits and become more physically active than you are right now.
Because we know change can be difficult, our YOW partners are working to provide community-based supports to make these changes easier. Diabetes Prevention Program (DPP) classes are one way to learn about healthy habits and how you can adapt your lifestyle to optimize health. Plan to attend the DPP orientation, March 6th at either 12:00 noon or 6 p.m. at the YMCA, 610 Stillwell Avenue in Tillamook. You have nothing to lose (but weight) and everything to gain (in health)!
Continue to follow us in the Headlight-Herald each week to learn more about local resources available to you and your family. Visit our website at tillamookcountyhealthmatters.org or download the app, Tillamook County YOW, for additional community-based wellness resources and information.